 Whatever relief providers felt after the recent CMS MACRA Pick Your Pace announcement, don’t be fooled. CMS has not, it seems, backed off its goals of pushing providers toward Risk, nor the interim and final quotas for participation. To the contrary—the announcement pointedly suggested that providers consider joining a risk-based Alternative Payment Model (APM) in 2017.
Whatever relief providers felt after the recent CMS MACRA Pick Your Pace announcement, don’t be fooled. CMS has not, it seems, backed off its goals of pushing providers toward Risk, nor the interim and final quotas for participation. To the contrary—the announcement pointedly suggested that providers consider joining a risk-based Alternative Payment Model (APM) in 2017.
But here’s the bigger issue: most existing ACOs have failed to meet cost targets, and the risk of losses for risk-based APMs will fall back on the participating providers. MACRA Pick your Pace should not be a time of rest. You should run, not walk, to start focusing on Performance Improvement, so you can avoid those losses before you are fully at risk.
Performance Improvement: Metrics Don’t Work Magic
Coming out of the HEDIS, Core Measure, Meaningful Use and PQRS era, everyone has gone mad about scoring physicians. If you ask most health care organizations about their Performance Improvement programs, the majority will tell you about their measures and metrics, and how physicians get rewarded by meeting them.
I am not saying that measurement is unimportant, because it is very important. But there are a few problems with substituting performance measurement for a real Performance Improvement program.
First, performance measurement isn’t usually about outcomes or even patients, but about processes that are done or not done. Those processes may be significant, but any measure is only tangentially related to cost, which means that you’re not getting a lot of cost reduction for the effort. So it won’t help you with the coming of Risk. And, the future of MACRA, as stipulated by CMS, is focused on outcome and not process measures.
Second, performance measurement has inherent flaws. The data are often inaccurate or incomplete. And the focus on aggregate results is overwhelmingly negative, alienating providers rather than creating collegiality toward achieving goals. Scoring creates a search for the bad apples, not for the good ones, and physicians understand this and reject it.
Third, although scoring providers based on metrics is technically an “intervention” in Performance Improvement jargon, it usually is not actionable. There are too many missing pieces—why certain tests were not done, why a readmission occurred, as two examples. Without understanding more, providers can’t fix it.
Bottom line: performance measurement and Performance Improvement are not the same. If you want results that will protect you in a risk-based APM, activities must be focused on patients and not just provider behavior.
How Performance Improvement is Distinct
Improving performance requires much more than assessments of compliance with performance measures and targets. It involves a process of inquiry to address deficiencies or specific areas of improvement, plus activities and interventions that will engineer change.
APMs that are successful will need scores of activities to improve performance, not just a handful. The causes for over-expenditures will drive the activities, but the data will require further discovery and validation to explain the hidden reasons for overuse of resources or poor outcomes. Such data will not be found in EHRs and will require either provider or patient input, or both.
Unlike static values of measurements, Performance Improvement must be value-driven and dynamic, always ready to tailor efforts to what is working—and redirect from what is not.
Five Keys for MACRA Performance Improvement Activities
- Create a participatory process and provider-led Interventions. “Participatory” means that clinicians are involved in providing input to planned interventions. Even better—facilitate their priorities for clinical care. If you give physicians the incentive and power to improve performance, rather than achieve compliance, you will foster greater innovation, as well as positive results.
- Use Quality Resource Use Reports (QRURs) to determine target areas for cost performance activities. Although CMS holds all of the data for its Resource Use calculations, providers get retrospective data through CMS. The data are rich in information; practice-based QRURs should be a significant source of information for their APMs, so that the APM can support the practice in Performance Improvement.
- Test activities in groups or on a small population prior to rollout across the organization. Most activities should be pilots, but APMs tend to decide and then rollout before seeing what works. Case in point: intensive case management, with effectiveness highly dependent on the buy-in of practices and patient populations.
- Aim for a positive process in clinical Performance Improvement. Most activities are focused on what is going wrong, but the tone must be positive—especially in outcomes. This is where reputations are built, and physicians can be both proud and guarded. Plus, why some patients improve and some do not really is a mystery. Therefore, make it a discovery process rather than a punitive ordeal to figure out why outcome trends are improving—or not. Non-traditional approaches will work well here.
- Cultivate shared decision-making with patients. Even if you have a CMS-attributed pool of patients in your APM, recognize that these patients are not “yours.” In order to control resources, you will need to establish a trust relationship that will result in appropriate use of services and better patient results. The best way is to embrace a shared decision-making model, paired with coaching your clinicians to make this work effectively through better communication skills and sharing of treatment benefits and harms.
Designing effective performance improvement activities will require innovation—as well as a serious leadership effort to make believers out of physicians who have been injured by past actions! This is the year to be brave and audacious, while you still have the ability to make mistakes.
Founded in 2002, ICLOPS has pioneered data registry solutions for performance improvement in health care. Our industry experts provide comprehensive Solutions that help you both report and improve your performance. ICLOPS is a CMS Qualified Clinical Data Registry.
Contact ICLOPS for a Discovery Session
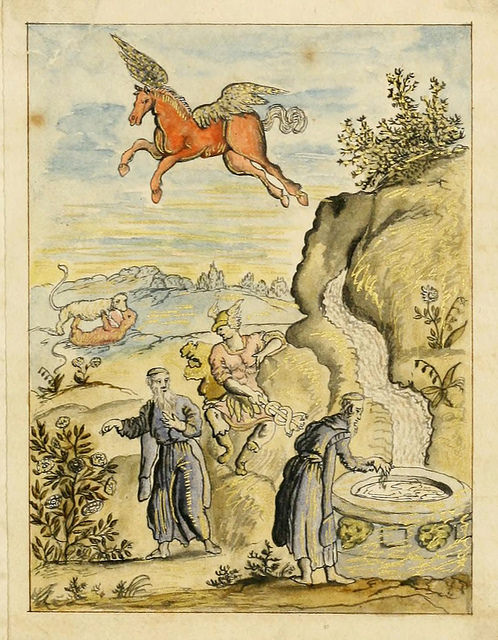
Image Credit: Manly Palm Hall collection of alchemical manuscripts, 1500-1825, Getty Research Institute.






